6650 Frankford Ave
Philadelphia, PA 19135
When the fibrous tissue on the sole that connects the heel with the front of the foot (plantar fascia) becomes damaged and inflamed, this is known as plantar fasciitis. Plantar fasciitis can also cause tense muscles in other parts of the foot and calf. Sometimes stretches can ease some of this tension and discomfort in these muscles as well as the plantar fascia. Simple calf stretches are a good place to start. To get a good stretch in the affected foot, place it behind you—flat on the ground—with the leg and knee straight. The other leg should be bent in front of you with that foot also lying flat, and your hands placed against a wall in front of you. Hold that position for 10 seconds and then release. You should feel an easy stretch in the calf and heel of the affected foot. Rolling a foam roller or ball back and forth under the affected foot while seated can also provide a good stretch in the foot. For another gentle calf stretch, sit on a chair and either curl a towel on the floor or pick up marbles with your toes. If your plantar fasciitis does not improve or is severe, a podiatrist can offer many solutions to treat it.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact John M. Fanelly, DPM from Northeast Philadelphia. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
How Can It Be Treated?
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our office located in Philadelphia, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
 Orthotics are special shoe inserts that are designed to help correct a variety of foot related issues by relieving pressure or realigning the feet. They can also help reduce pain in the feet, knees, and lower back. There are three common types of orthotics known as soft, rigid, and semi-rigid. Soft orthotics are made to provide extra cushioning while the foot is planted on the ground. Semi-rigid orthotics, which are often used on flat feet, are designed to provide both cushioning and stability. Meanwhile, rigid orthotics are designed to provide stability and to help prevent movements that can cause pain. Patients who believe that orthotics are right for them should visit a podiatrist. A podiatrist will be able to customize an orthotic and tailor it to your needs.
Orthotics are special shoe inserts that are designed to help correct a variety of foot related issues by relieving pressure or realigning the feet. They can also help reduce pain in the feet, knees, and lower back. There are three common types of orthotics known as soft, rigid, and semi-rigid. Soft orthotics are made to provide extra cushioning while the foot is planted on the ground. Semi-rigid orthotics, which are often used on flat feet, are designed to provide both cushioning and stability. Meanwhile, rigid orthotics are designed to provide stability and to help prevent movements that can cause pain. Patients who believe that orthotics are right for them should visit a podiatrist. A podiatrist will be able to customize an orthotic and tailor it to your needs.
If you are having discomfort in your feet and would like to try orthotics, contact John M. Fanelly, DPM from Northeast Philadelphia. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Are Orthotics?
Orthotics are inserts you can place into your shoes to help with a variety of foot problems such as flat feet or foot pain. Orthotics provide relief and comfort for minor foot and heel pain but can’t correct serious biomechanical problems in your feet.
Over-the-Counter Inserts
Orthotics come in a wide variety of over-the-counter inserts that are used to treat foot pain, heel pain, and minor problems. For example, arch supports can be inserted into your shoes to help correct overarched or flat feet, while gel insoles are often used because they provide comfort and relief from foot and heel pain by alleviating pressure.
Prescription Orthotics
If over-the-counter inserts don’t work for you or if you have a more severe foot concern, it is possible to have your podiatrist prescribe custom orthotics. These high-quality inserts are designed to treat problems such as abnormal motion, plantar fasciitis, and severe forms of heel pain. They can even be used to help patients suffering from diabetes by treating foot ulcers and painful calluses and are usually molded to your feet individually, which allows them to provide full support and comfort.
If you are experiencing minor to severe foot or heel pain, it’s recommended to speak with your podiatrist about the possibilities of using orthotics. A podiatrist can determine which type of orthotic is right for you and allow you to take the first steps towards being pain-free.
If you have any questions please contact our office located in Philadelphia, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
A bunion is a common foot deformity characterized by a bony bump that forms at the base of the big toe joint. The bump can become inflamed, red, swollen, and painful. It also pushes the big toe out of alignment, so that it is tilted toward the smaller toes instead of pointing straight ahead. Bunions progressively worsen without treatment, and surgery is often the only option to permanently remove them. That said, there are many things to consider prior to making the decision to operate. Certain underlying health conditions, such as diabetes, rheumatoid arthritis, and gout, can increase the risk of complications from surgery. It is also important to think about your lifestyle. Do you intend to wear high heels, exercise, or stand for prolonged periods of time? These factors can help your podiatrist determine if bunion surgery is the right treatment option for you. For more information about bunions, please consult with a podiatrist.
If you are suffering from bunions, contact John M. Fanelly, DPM of Northeast Philadelphia. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
A bunion is formed of swollen tissue or an enlargement of boney growth, usually located at the base joint of the toe that connects to the foot. The swelling occurs due to the bones in the big toe shifting inward, which impacts the other toes of the foot. This causes the area around the base of the big toe to become inflamed and painful.
Why Do Bunions Form?
Genetics – Susceptibility to bunions are often hereditary
Stress on the feet – Poorly fitted and uncomfortable footwear that places stress on feet, such as heels, can worsen existing bunions
How Are Bunions Diagnosed?
Doctors often perform two tests – blood tests and x-rays – when trying to diagnose bunions, especially in the early stages of development. Blood tests help determine if the foot pain is being caused by something else, such as arthritis, while x-rays provide a clear picture of your bone structure to your doctor.
How Are Bunions Treated?
If you have any questions, please feel free to contact our office located in Philadelphia, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
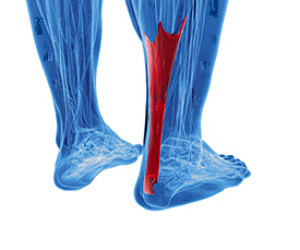 When the Achilles tendon, which is the large tendon on the back of the ankle connecting the calf to the heel bone, becomes inflamed, Achilles tendonitis occurs. Achilles tendonitis may not come from any particular trauma, but instead, the pain gradually worsens over time. Most of the time, pain from Achilles tendonitis is worse in the morning and after long periods of rest, and the pain lessens throughout the day. The most common cause of Achilles tendonitis is over-pronation which is when the arch of the foot flattens upon bearing weight and puts stress on the tendon. Other factors that can lead to Achilles tendonitis include poorly fitting shoes, poor stretching, trauma or a shortened tendon. Patients who are experiencing symptoms of Achilles tendonitis should consult a podiatrist, because it can eventually lead to a painful rupture of the tendon.
When the Achilles tendon, which is the large tendon on the back of the ankle connecting the calf to the heel bone, becomes inflamed, Achilles tendonitis occurs. Achilles tendonitis may not come from any particular trauma, but instead, the pain gradually worsens over time. Most of the time, pain from Achilles tendonitis is worse in the morning and after long periods of rest, and the pain lessens throughout the day. The most common cause of Achilles tendonitis is over-pronation which is when the arch of the foot flattens upon bearing weight and puts stress on the tendon. Other factors that can lead to Achilles tendonitis include poorly fitting shoes, poor stretching, trauma or a shortened tendon. Patients who are experiencing symptoms of Achilles tendonitis should consult a podiatrist, because it can eventually lead to a painful rupture of the tendon.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact John M. Fanelly, DPM of Northeast Philadelphia. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
Rupture Symptoms
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
If you have any questions please feel free to contact our office located in Philadelphia, PA . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.